Calls for a ban on veterinary use of colistin, also used as a last line of treatment in human medicine, along with a new study showing growing resistance to the last line antibiotic group carbapenems, came as the World Health Organization (WHO) held its first Antibiotics Awareness Week.
The livestock study, from China, revealed the discovery of the mcr-1 gene, which allows a range of common bacteria, including Escherichia coli, to become resistant to the polymixin class of antibiotics, which includes colistin, used in poultry and other livestock primarily to treat E coli and Salmonella gastrointestinal tract infections.
The gene was found by chance during routine testing of animals destined for consumption, leading the researchers to conduct more widespread testing.
Bacteria samples were collected from pigs at slaughter and from retailed chicken and pork between 2011 and 2014. Bacterial samples from patients with infections at two hospitals in Guangdong and Zheidong were also studied.
The researchers found the gene in 166 out of 804 animals and in 78 of 523 raw meat samples. They also found it in 16 E coli and Klebsiella penumoniae samples from 1,322 patients.
“These are extremely worrying results,” said Professor Jian-Hua Liu, from the South China Agricultural University, and author of the report.
“Our results reveal the emergence of the first polymixin resistance gene that is readily passed between common bacteria such as E coli and K pneumoniae, suggesting the progression from extensive resistance to pandrug resistance is inevitable.”
No more veterinary colistin use?
In response to the findings, there were immediate calls for colistin use on farms to be severely limited or stopped altogether to slow livestock antibiotic resistance progression.
A statement from the UK Responsible Use of Medicines Alliance (RUMA), however, noted that use of antimicrobials in the Chinese pig herd is not normally under veterinary control. Trade in pig meat was unlikely to spread the bacteria, it continued, however transfer by humans posed a greater risk, particularly via trade and tourism.
The statement pointed to other recent research looking at attribution of extended-spectrum beta lactamase resistance from food to man, which has shown that man to man is the major contributor -- not poultry, pig or other livestock to man -- due to hospital care spread of bacteria carrying resistance genes.
More barriers fall
The Chinese publication came after the release of European Centre for Disease Prevention and Control (ECDC) survey results revealing that the spread of carbapenemase-producing Enterobactericae (CPE) in the EU is continuing, with eight countries reporting an interregional spread, and three an endemic situation. In these three countries, most hospitals are reportedly seeing patients that cannot be treated with carbapenems – a last line antibiotic group.
Antibiotic resistance increasing daily
Vytenis Andriukailis, European Commissioner for Health and Food Safety said: “The ECDC results show that the threat of antibiotic resistance is increasing day by day. If left unchecked, it has the capacity to run the clock back on medicine by a hundred years.”
The European survey, released on the region’s eighth Antibiotics Day, also found that resistance continued to rise for most bacteria and antibiotics under surveillance.
A positive finding, however, was that there was a significant decrease in antibiotic consumption in five European countries, yet antibiotic use in the hospital sector, overall and for carbapenems, is still increasing.
Carbapenems are not authorized for use in poultry or other livestock production, leaving little doubt as to where resistance emerged.
Livestock production the major culprit?
As part of WHO Antibiotics Awareness Week and its new campaign “Antibiotics: Handle with care,” the organization released survey results on public awareness of antibiotic resistance.
Of the 10,000 people questioned across 12 countries, almost 75 percent believed livestock should be given fewer antimicrobials.
The survey, however, highlighted the major problems that exist within human antibiotic prescribing, compliance and understanding.

The World Health Organization points out that there are various ways in which antibiotic resistance can develop.
Seventy-six percent of respondents believed resistance occurs when the body becomes resistant to antibiotics, while two-thirds thought they would not be at risk from drug-resistant bacteria if they took antibiotics as prescribed.
Prescription, attitudes and compliance vary greatly from country to country.
In China, for example, where 83 percent of respondents said livestock farmers should use fewer antibiotics, 57 percent of respondents reported taking antibiotics within the past six months. Seventy-four percent said they had been doctor or nurse prescribed, with 5 percent having bought them online.
More than half of respondents believed they should stop taking their antibiotics when they felt better.
“The findings of this survey point to the urgent need to improve understanding around antibiotic resistance,” said Dr. Keiji Fujuda, special representative of the director general for antimicrobial resistance. “One of the biggest health challenges of the 21st century will require global behavior change by individuals and societies.”
One Health the answer
In response to Europe’s awareness day, the European Platform for the Responsible Use of Medicines in Animals (EPRUMA), which comprises agricultural associations, argued that more should be done to develop science-based resources to prevent and control disease in humans and animals.
The right legal framework also needs to be put in place for the provision of innovative animal medicines, including veterinary antibiotics, and diagnostics, to help treat disease efficiently and work toward tackling resistance, it added.
A similar view came from veterinary medicines association IFAH-Europe.
“Actions to reduce resistance need to be taken in a One Heath context with all sectors concerned combining efforts to develop science-based solutions. The main objective should be to reduce resistance to antibiotics, not simply to reduce antibiotic use,” IFAH-Europe secretary general Roxane Feller said.
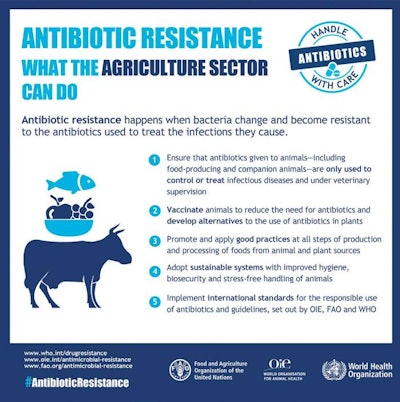
As part of the Antibiotics: Handle With Care campaign, WHO is offering specific advice to the livestock sector on antibiotic use.
To learn more, read:
Antibiotics strategies must target resistance, not use

















