Mycotoxins are always present in animal feeds, although at varying levels, and affect various systems in poultry, such as the gastrointestinal tract (GIT) and visceral organs.
They produce a variety of diseases, collectively called "mycotoxicoses," directly or in combination with other primary stressors, such as pathogens. Mycotoxicoses are characterized by symptoms including lesions, which can be used to clinically diagnose the presence of mycotoxins. These lesions, however, may not be caused by mycotoxins alone. They can be the result of diverse nutritional, management and pathogenic conditions, making it important to differentially diagnose, i.e., to distinguish a disease or condition from others exhibiting similar signs, before arriving at a conclusion.
Mycotoxic lesions in poultry
The GIT is the first system exposed to the effects of mycotoxins upon ingestion. The T-2 toxin (T-2), HT-2 toxin, deoxynivalenol (DON), monoacetoxyscirpenol (MAS) and diacetoxyscirpenol (DAS) from the Fusarium-derived trichothecenes group and cyclopiazonic acid (CPA) from either Aspergillus flavus or Penicillium spp. are the primary mycotoxins that affect the GIT.
These mycotoxins are capable of causing oral lesions, crop necrosis, gizzard erosion, proventriculitis, inflammation of epithelial mucosa and intestinal hemorrhage.
The T-2 toxin and DAS have a more caustic effect, compared to other toxins in the group, and produce lesions in the mouth (tongue, beak, palate), as well as erosion in gizzard. The gizzard is also the primary organ affected by DON, which increases gizzard weight and gizzard erosion when levels are high.
Other mycotoxins that and cause gizzard ulcers include moniliformin and fumonisin B1 and B2. CPA affects the mucosa of proventriculus and causes proventriculilits. These mycotoxins dissolve the protoplasm of cells in the mucosa, while saliva in the mouth facilitates their adherence to the mucosa. Upon their absorption through the intestines, these mycotoxins translocate into the circulatory system and return to the oral cavity through saliva, again causing secondary lesions in the mouth and possibly in the gizzard.
Differential diagnosis
There are a variety of conditions of either non-pathogenic or pathogenic origin that are typified by lesions in the GIT. Most conditions of non-pathogenic etiology are due to either nutritional or management causes, while the pathologic etiologic agents include living organisms such as fungi, protozoa, bacteria and viruses.
Some of the conditions that should be ruled out when considering mycotoxicoses are:
1. Nutritional conditions
- Copper
- Zinc
- Choline chloride
- Sulfur amino acids
- Vitamins (A, E, B6, biotin)
- Biogenic amines
- Fish meal
- Feed structure (mash/pellet)
- Feed composition (fiber content)
2. Management conditions
- Quaternary Ammonium Compounds (QAC)
- Starvation
- Hatching stress
- Debeaking
3. Pathogenic conditions
- Thrush/Candidiasis
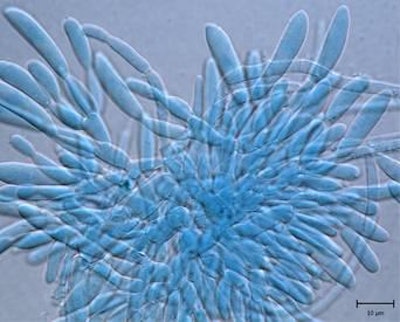
- Pseudomembranous Ingluvitis/Aspergillosis
- Helminthiasis
- Histomoniasis/Blackhead disease
- Coccidiosis
- Clostridium colinum infection
- Clostridium perfringens infection
- Avian Poxvirus
- Avian Adenovirus
- Avian Reovirus
It is not easy to establish a differential diagnosis for the agents causing lesions in the GIT, such as an oral lesion, gizzard erosion, proventriculitis and intestinal necrosis. However, it is theoretically possible to microscopically differentiate the lesions caused by pathogenic agents from those of a non-pathogenic etiology.
Pathogenic etiologic agents capable of causing lesions in the GIT are characterized by marked lymphoid infiltration, which would not be possible to detect in their absence.
Among the viral agents listed, the localization of infiltration varies according to the type of virus, as well as the presence of typical viral lesions in other organs.
In the case of reovirus and adenovirus, the infiltration is present in the muscular wall of the organ and not in the gland, as it occurs in the lesions produced by Marek's disease. Another important difference in the lesions caused by Marek's disease is the presence of a lymphoid infiltrate in the serosa layer of the nerves in the external wall of the proventriculus.
When GIT lesions are detected in the field, an effective differential diagnosis will help to determine which control measures should be taken. Under commercial poultry farming conditions, it is difficult to associate these lesions with only one etiologic agent, since they represent the result of the combination of several agents including mycotoxins, which are more likely to act along with a major causative agent.
Several published experiments have demonstrated potentiation of the negative effects (not only in terms of lesions in GIT) caused by the association between mycotoxins and the agents listed here, such as biogenic amines, gizzerosine, Aspergillus fumigatus, Clostridium spp., and reovirus, etc. Hence, there is no doubt that feed contamination with mycotoxins plays an important role in causing these lesions in the GIT. Routine testing of feed samples for mycotoxins as well as an understanding of the effects of mycotoxicoses would be a good start.
Mycotoxin risk management in poultry
A proper "Mycotoxin Risk Management" tool is crucial to prevent poultry from the hazardous effects of mycotoxins.
Mineral binders are commonly supplemented through feed to bind/adsorb various mycotoxins. However, trichothecenes, such as DON and T-2, have the lowest adsorption efficacy compared to polar mycotoxins, such as aflatoxins. As not all mycotoxins can be adsorbed by a mineral binder, different strategies have to be used to counteract mycotoxins with different properties.
Another critical point to consider is that not all binders are the same and will exhibit varying adsorption efficacy depending on their origin such as inorganic or organic, composition, surface area, etc.
When it comes to non-adsorbable mycotoxins, biotransformation is the major strategy that needs to be followed, where microbes/enzymes alter the structure of mycotoxins in order to render them as non-toxic metabolites.
Bioprotection is an additional strategy in which plant and algae extracts are used to provide a hepato-protective effect and to overcome the immune suppression caused by mycotoxins, respectively. Therefore, a combination of multiple strategies (adsorption + biotransformation + bioprotection) should be employed to counteract multiple mycotoxin challenges and mycotoxicoses.
















