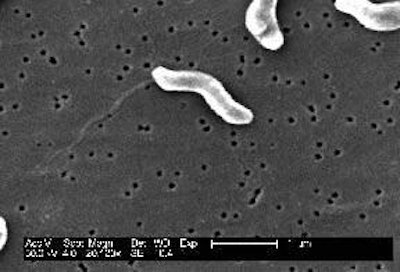
As pork is one of the main meats consumed in most countries, it features strongly in national and international food safety controls. Salmonella is the better known of the bacterial risks among pig producers, but a possible contamination by Campylobacter must also be considered because its bacteria represent an important zoonotic agent.
Zoonoses are diseases that can be transmitted from animals to humans. According to the World Health Organisation, Campylobacter is the leading cause of bacterial diarrhoea in people around the world. A recent European review showed that it was on a strong trend of growth, cases increasing by over 30% between 2004 and 2005.
Statistics on zoonoses published by the European Commission in 2006 confirmed salmonellosis and campylobacteriosis as the most common food-borne diseases affecting people in the then 25 European Union (EU) countries, with the incidence of Campylobacter averaging over 47 cases for every 100 000 people.
Apart from the possibility of affects on the consumer's digestive system, scientific concerns are heard about secondary problems including an irreversible disease of the nervous system, the Guillain Barré syndrome. More alarming still is the resistance common among these bacteria to the antibiotics used in treating human patients. European data refer to up to half of all Campylobacter infections in humans as being resistant to fluoroquinolones, tetracyclines, quinolones and penicillins. In some countries the majority of Campylobacter isolates from poultry, pigs and sheep were resistant to quinolones and fluoroquinolones.
Fewer found in pigs
Slaughter surveys in the EU in 2005 revealed that samples testing positive for Campylobacter were collected from just under 80% of pig carcases, compared with 91% of poultry and slightly more than 64% of cattle. However, the data do not prove that a direct link exists between the Campylobacter carried by pigs and the antibiotic-resistant campylobacteriosis encountered in human medicine. Most studies identify poultrymeat as the main source of the bacteria affecting humans, although some have been found in pork and beef.
Fresh information on the subject emerged from French research described recently in the Journées de la recherche porcine the annual French symposium about pork production methods.
Julien Fosse (from the national veterinary school of Nantes) and his colleagues analysed the 35 biological dangers that pork can transmit to consumers. Of these, he explained, 12 infections have the potential to be passed through eating the food. Pork contributes to about 10% of the zoonotic incidents.
Microbes scored for danger
The research group led by Dr Fosse rated the biological dangers for the severity of their possible effect on humans. This allocated the highest score on gravity to the organisms Listeria monocytogenes and Clostridium botulinum. But ratings shifted to Salmonella enterica, Yersinia enterocolitica enterica, Yersinia enterocolitica and to the types of Campylobacter resistant to temperature (mainly C. jejuni and C. coli) when frequency of the various infections was considered.
Unfortunately, these dangers are not detectable by the classic controls followed at the slaughterhouse. Their presence can be confirmed only by a more detailed examination of the meat. The slaughterhouse therefore has little information to consider for its Hazard Analysis and Critical Control Point hazard-control analyses. Alternative signs might be sought at farm level, but that is also proving to be difficult.
Presentations to the French research meeting noted that the pig is an asymptomatic carrier of Campylobacter. It hosts the bacteria, but develops no external signs of infection. Neither eating behaviour nor reproductive results show any change.
Tracking back Campylobacter as causing diarrhoea in humans, the Nantes team also looked at contamination inside the farm. This is mainly horizontal, commented Mily Leblanc Maridor (ENV/Inra) and colleagues. It spreads rapidly through manure from infected to non-infected pigs, which in turn excrete the bacteria. Solid walls rather than rails between groups of pigs is a useful way of reducing this faecal transfer in the grow-finish house.
Martine Denis from food safety agency AFSSA in Ploufragan, France, reported its investigation into 133 isolates of Campylobacter coli collected in 2003 from a study of cases in Brittany (north-west France) with local organisations RFLP and PFGE. She indicated that 65 of these isolates came from pigs and 56 from poultry, leaving 12 isolated from human campylobacteriosis.
No single type common to the 3 sources could be detected. But an analysis of genetic similarities involving 80% of the isolates made it possible to group them into 19 general categories. It demonstrated 3 cases in which poultry isolates belonged to groups containing a human isolate. Pig isolates were always in groups that consisted exclusively of isolates from pigs.
It could be a highly significant finding, the speakers suggested. Poultry and pigs each appear to have their own genotype regarding the bacteria they carry. Whereas those on poultrymeat can and do pass to humans, it seems that the Campylobacter bacteria from pigs are rarely responsible for human campylobacteriosis. PIGI

















